06
What Are Dental Cavitations?
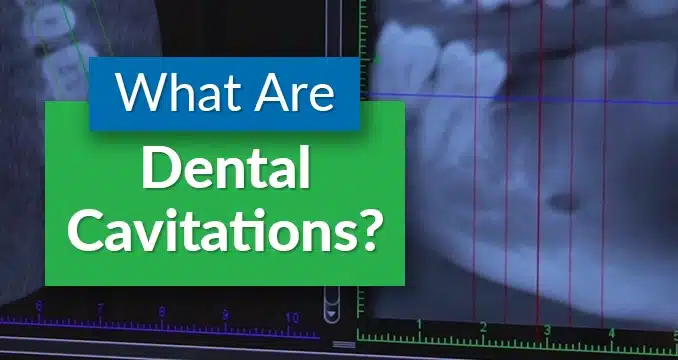
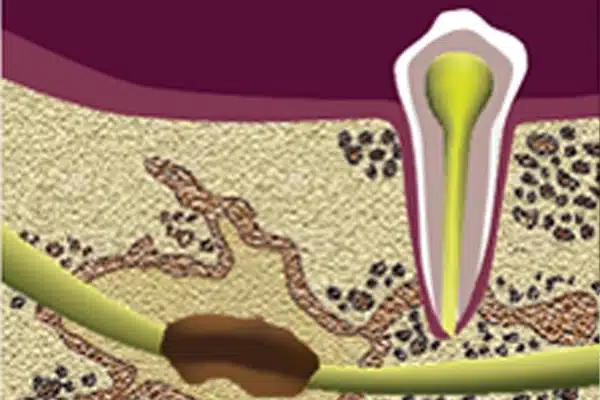
If the area where a tooth is removed doesn’t heal properly, a hole persists in the bone. This hole is called a cavitation. According to this research paper from the IAOMT website, a cavitation can be identified by the presence of necrotic, or dying bone in the medullary component of the jawbone.
In this chapter, we discuss where dental cavitations come from and the best way to treat them.
What Are Dental Cavitations and Why Are They a Problem? Understanding Chronic Inflammation
Dental cavitations, often overlooked but potentially significant, are areas of unhealed bone tissue in the jawbone, also known as chronic ischemic jawbone disease. When a tooth is removed, the bone surrounding it may fail to heal properly, resulting in a cavity-like void that disrupts normal blood flow and compromises the health of surrounding bone cells. Dental cavitations are found in areas where the teeth have been removed, often in the wisdom tooth area.
These cavitations can lead to various complications, ranging from localized issues like tooth abscesses to more systemic health concerns such as chronic facial pain and chronic inflammation. Understanding the origins and implications of dental cavitations is crucial for navigating oral health and making informed decisions about oral surgery.
In a large majority of cavitation cases, people have one or more areas where a wisdom or other tooth has been removed, and an unhealed cavity in the bone has remained.
Because the bone is unhealed, there isn’t blood flow to the area. This leads to further bone decay and a larger area of cavitation. Harmful bacteria and unhealthy bone tissue can accumulate in these areas, exacerbating the problem.
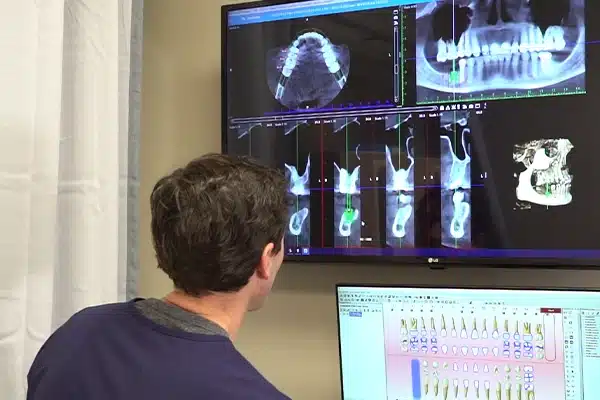
Any dental cavitation, no matter how “hidden”, can be found on a dental-specific Cone Beam CT scan, by looking for decreased bone density.
Do keep in mind that only specially trained dentists are able to read the CT scan and look for areas of decreased bone density. If you’re interested in an exam to see if you have a cavitation, make sure it’s with a dentist who meets these qualifications.
These cavitations are like toxic sinkholes. They contain microbes that impair the function of some systems in the body, particularly the hormone and energy production systems, as well as gut function, heart and joint health.
That’s right, something going on in your jaw bone could be the reason you feel like you need a jump start just to get out of bed!
These toxic microbes can slow you down, leading to fatigue, brain fog, and other energy-related problems. Research shows dental cavitations are linked to Chronic Fatigue Syndrome.
The difficulty with these and other hormone, gut or heart symptoms, however, is that they may manifest themselves quickly or over years. This has a lot to do with immune system strength. This is why many cavitations go unnoticed and people become accustomed to living their lives fatigued, or with other chronic health problems without ever knowing the reason why.
There is current research in Germany also showing a correlation between these bone cavitations and other serious systemic diseases like:
Cancer
Autoimmune disease
Inflammatory disease, including heart disease and arthritis
Brain and nerve problems
How Dental Cavitations Are Treated

The truth is that there are few dentists who know how to diagnose bony cavitations properly – and even fewer who know how to treat them!
You want to make sure dental cavitations are dealt with correctly, so it’s highly recommended that you choose a dental surgeon with significant experience removing the dead bone and disinfecting the site, as well as stimulating the area to heal and grow new bone.
This is a very specialized surgery that needs to be done with care, caution, and precision. Ozone therapy is often used to eliminate anaerobic bacteria and potent toxins within the cavitation lesions, promoting a clean and sterile environment for healing.
Stacy's Story
Stacey was sick and didn’t know why. She was in her early 30s and had to quit a career she loved and move back in with her parents. She spent most of her days in bed, waking up late and lacking the energy to even get out of bed.
She gained unexplained weight, had chronic energy issues, and her mother was afraid Stacey might not make it through these challenges.
They had been to so many doctors, tried so many things, and nothing had made a significant improvement in her health or her energy. She was eventually referred to my office to see if she might have bony cavitations. Before proceeding, we reviewed her dental and medical history to determine any possible causes of the bone lesion.
On a Cone Beam CT scan, we found areas of cavitated bone in all of her wisdom tooth removal sites, indicative of neuralgia inducing cavitational osteonecrosis. She also had an infected root canal tooth.
In just one surgical appointment, all of the cavitation areas were opened up, cleaned, and sterilized. Then a stem cell-containing product from her own blood was placed into the areas to encourage growth and nourishment. The root canal tooth was also removed and an immediate ceramic implant was placed.
She reported feeling more like herself the same afternoon of the surgery, and the next day her mother found her doing dishes, rather than just in bed like she’d been the last several years.
Stacey started walking and is now traveling eight miles on foot each day. She just left on a long-awaited trip to China that she never thought she would be able to take. It turns out that discovering she had dental cavitations, and finding an expert who could treat them correctly, saved her life.
Referenced Articles:
- International Academy of Oral Medicine and Toxicology. (n.d.). IAOMT jawbone cavitations position paper. Retrieved from https://iaomt.org/resources/position-papers/iaomt-jawbone-cavitations-position-paper/
- Lechner J, von Baehr V. RANTES and fibroblast growth factor 2 in jawbone cavitations: triggers for systemic disease?. Int J Gen Med. 2013;6:277-290. Published 2013 Apr 22. doi:10.2147/IJGM.S43852
- Lechner J, von Baehr V. Chemokine RANTES/CCL5 as an unknown link between wound healing in the jawbone and systemic disease: is prediction and tailored treatments in the horizon?. EPMA J. 2015;6(1):10. Published 2015 May 6. doi:10.1186/s13167-015-0032-4
- Lechner J, von Baehr V. Hyperactivated Signaling Pathways of Chemokine RANTES/CCL5 in Osteopathies of Jawbone in Breast Cancer Patients-Case Report and Research. Breast Cancer (Auckl). 2014;8:89-96. Published 2014 May 21. doi:10.4137/BCBCR.S15119
- Lechner J, Huesker K, Von Baehr V. Impact of Rantes from jawbone on Chronic Fatigue Syndrome. J Biol Regul Homeost Agents. 2017;31(2):321-327.
- Lechner J, von Baehr V, Schick F. RANTES/CCL5 Signaling from Jawbone Cavitations to Epistemology of Multiple Sclerosis – Research and Case Studies. Degener Neurol Neuromuscul Dis. 2021;11:41-50. Published 2021 Jul 5. doi:10.2147/DNND.S315321
- Lechner J, Schmidt M, von Baehr V, Schick F. Undetected Jawbone Marrow Defects as Inflammatory and Degenerative Signaling Pathways: Chemokine RANTES/CCL5 as a Possible Link Between the Jawbone and Systemic Interactions?. J Inflamm Res. 2021;14:1603-1612. Published 2021 Apr 21. doi:10.2147/JIR.S307635
- Lechner J, Rudi T, von Baehr V. Osteoimmunology of tumor necrosis factor-alpha, IL-6, and RANTES/CCL5: a review of known and poorly understood inflammatory patterns in osteonecrosis. Clin Cosmet Investig Dent. 2018;10:251-262. Published 2018 Nov 9. doi:10.2147/CCIDE.S184498